Can Diet Affect The Health Of Our Planet?
Author: Dr. Stephen Chaney
 Earth Day was yesterday. So, it is time for my annual reminder that what you eat affects a lot more than just your health. It affects the health of our planet. Once again, it’s time to ask yourself, “Is my diet destroying the planet?
Earth Day was yesterday. So, it is time for my annual reminder that what you eat affects a lot more than just your health. It affects the health of our planet. Once again, it’s time to ask yourself, “Is my diet destroying the planet?
This is not a new question, but a recent commission of international scientists has conducted a comprehensive study into our diet and its effect on our health and our environment. Their report (W. Willet et al, The Lancet, 393, issue 10170, 447-492, 2019) serves as a dire warning of what will happen if we don’t change our ways.
The commission carefully evaluated diet and food production methods and asked three questions:
- Are they good for us?
- Are they good for the planet?
- Are they sustainable? Will they be able to meet the needs of the projected population of 10 billion people in 2050 without degrading our environment.
The commission described the typical American diet as a “lose-lose-lose diet”. It is bad for our health. It is bad for the planet. And it is not sustainable.
In its place they carefully designed their version of a primarily plant-based diet they called a “win-win-win diet”. It is good for our health. It is good for the planet. And it is sustainable.
In their publication they refer to their diet as the “universal healthy reference diet” (What else would you expect from a committee?). However, it has become popularly known as the “Planetary Diet”.
I have spoken before about the importance of a primarily plant-based diet for our health. In that context it is a personal choice. It is optional.
However, this report is a wake-up call. It puts a primarily plant-based diet in an entirely different context. It is essential for the survival of our planet. It is no longer optional.
If you care about our environment…If you care about saving our planet, there is no other choice.
How Was The Study Done?
The publication (W. Willet et al, The Lancet, 393, issue 10170, 447-492, 2019) was the report of the EAT-Lancet Commission on Healthy Diets from Sustainable Food Systems. This Commission convened 30 of the top experts from across the globe to prepare a science-based evaluation of the effect of diet on both health and sustainable food production through the year 2050. The Commission included world class experts on healthy diets, agricultural methods, climate change, and earth sciences. The Commission reviewed 356 published studies in preparing their report.
Can Diet Affect The Health Of Our Planet?
 When they looked at the effect of food production on the environment, the Commission concluded:
When they looked at the effect of food production on the environment, the Commission concluded:
- “Strong evidence indicates that food production is among the largest drivers of global environmental change.” Specifically, the commission reported:
-
- Agriculture occupies 40% of global land (58% of that is for pasture use).
-
- Food production is responsible for 30% of global greenhouse gas emissions and 70% of freshwater use.
-
- Conversion of natural ecosystems to croplands and pastures is the largest factor causing species to be threatened with extinction. Specifically, 80% of extinction threats to mammals and bird species are due to agricultural practices.
-
- Overuse and misuse of nitrogen and phosphorous in fertilizers causes eutrophication. In case you are wondering, eutrophication is defined as the process by which a body of water becomes enriched in dissolved nutrients (such as phosphates from commercial fertilizer) that stimulate the growth of algae and other aquatic plant life, usually resulting in the depletion of dissolved oxygen. This creates dead zones in lakes and coastal regions where fish and other marine organisms cannot survive.
- About 60% of world fish stocks are fully fished and more than 30% are overfished. Because of this, catch by global marine fisheries has been declining since 1996.
- “Reaching the Paris Agreement of limiting global warming…is not possible by only decarbonizing the global energy systems. Transformation to healthy diets from sustainable food systems is essential to achieving the Paris Agreement.”
- The world’s population is expected to increase to 10 billion by 2050. The current system of food production is unsustainable.
 When they looked at the effect of the foods we eat on the environment, the Commission concluded:
When they looked at the effect of the foods we eat on the environment, the Commission concluded:
- Beef and lamb are the biggest contributors to greenhouse gas emissions and land use.
-
- The concern about land use is obvious because of the large amount of pastureland required to raise cattle and sheep.
-
- The concern about greenhouse gas emissions is because cattle and sheep are ruminants. They not only breathe out CO2, but they also release methane into the atmosphere from fermentation in their rumens of the food they eat. Methane is a potent greenhouse gas, and it persists in the atmosphere 25 times longer than CO2.
- The concern about greenhouse gas emissions is because cattle and sheep are ruminants. They not only breathe out CO2, but they also release methane into the atmosphere from fermentation in their rumens of the food they eat. Methane is a potent greenhouse gas, and it persists in the atmosphere 25 times longer than CO2.
The single most important thing we can do as individuals to reduce greenhouse gas emissions is to eat less beef and lamb. [Note: grass fed cattle produce more greenhouse gas emissions than cattle raised on corn because they require 3 years to bring to market rather than 2 years.]
-
- In contrast, plant crops reduce greenhouse gas emissions by removing CO2 from the atmosphere.
- In terms of energy use beef, lamb, pork, chicken, dairy, and eggs all require much more energy to produce than any of the plant foods.
- In terms of eutrophication of our lakes and oceans, beef, lamb, and pork all cause much more eutrophication than any plant food. Dairy and eggs cause more eutrophication than any plant food except fruits.
Eat Green
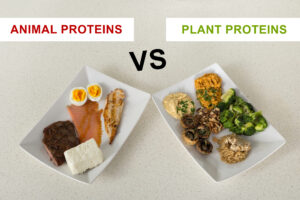
 In the words of the Commission: “[The Planetary Diet] largely consists of vegetables, fruits, whole grains, legumes, nuts, and unsaturated oils. It includes a low to moderate amount of seafood, poultry, and eggs. It includes no or a very low amount of red meat, processed meat, sugar, refined grains, and starchy vegetables.”
In the words of the Commission: “[The Planetary Diet] largely consists of vegetables, fruits, whole grains, legumes, nuts, and unsaturated oils. It includes a low to moderate amount of seafood, poultry, and eggs. It includes no or a very low amount of red meat, processed meat, sugar, refined grains, and starchy vegetables.”
When described in that fashion it sounds very much like other healthy diets such as semi-vegetarian, Mediterranean, DASH, and Flexitarian. However, what truly distinguishes it from the other diets is the restrictions placed on the non-plant portion of the diet to make it both environmentally friendly and sustainable. Here is a more detailed description of the diet:
- It starts with a vegetarian diet. Vegetables, fruits, beans, nuts, soy foods, and whole grains are the foundation of the diet.
- It allows the option of adding one serving of dairy a day (It turns out that cows produce much less greenhouse emissions per serving of dairy than per serving of beef. That’s because cows take several years to mature before they can be converted to meat, and they are emitting greenhouse gases the entire time).
- It allows the option of adding one 3 oz serving of fish or poultry or one egg per day.
- It allows the option of swapping seafood, poultry, or egg for a 3 oz serving of red meat no more than once a week. If you want a 12 oz steak, that would be no more than once a month.
This is obviously very different from the way most Americans currently eat. According to the Commission:
- “This would require greater than 50% reduction in consumption of unhealthy foods, such as red meat and sugar, and greater than 100% increase in the consumption of healthy foods, such as nuts, fruits, vegetables, and legumes”.
- “In addition to the benefits for the environment, “dietary changes from current diets to healthy diets are likely to substantially benefit human health, averting about 10.8-11.6 million deaths per year globally.”
What Else Did The Commission Recommend?
 In addition to changes in our diets, the Commission also recommended several changes in the way food is produced. Here are a few of them.
In addition to changes in our diets, the Commission also recommended several changes in the way food is produced. Here are a few of them.
- Reduce greenhouse gas emissions from the fuel used to transport food to market.
2) Reduce food losses and waste by at least 50%.
3) Make radical improvements in the efficiency of fertilizer and water use. In terms of fertilizer, the change would be two-fold:
-
- In developed countries, reduce fertilizer use and put in place systems to capture runoff and recycle the phosphorous.
-
- In third world countries, make fertilizer more available so that crop yields can be increased, something the Commission refer to as eliminating the “yield gap” between third world and developed countries.
4) Stop the expansion of new agricultural land use into natural ecosystems and put in place policies aimed at restoring and re-foresting degraded land.
5) Manage the world’s oceans effectively to ensure that fish stocks are used responsibly and global aquaculture (fish farm) production is expanded sustainability.
What we can do: While most of these are government level policies, we can contribute to the first three by reducing personal food waste and purchasing organic produce locally whenever possible.
What Does This Mean For You?
 If you are a vegan, you are probably asking why the Commission did not recommend a completely plant-based diet. The answer is that a vegan diet is perfect for the health of our planet. However, the Commission wanted to make a diet that was as consumer friendly as possible and still meet their goals of a healthy, environmentally friendly, and sustainable diet.
If you are a vegan, you are probably asking why the Commission did not recommend a completely plant-based diet. The answer is that a vegan diet is perfect for the health of our planet. However, the Commission wanted to make a diet that was as consumer friendly as possible and still meet their goals of a healthy, environmentally friendly, and sustainable diet.
If you are eating a typical American diet or one of the fad diets that encourage meat consumption, you are probably wondering how you can ever make such drastic changes to your diet. The answer is “one step at a time”. If you have read the Forward to my books “Slaying The Food Myths” or “Slaying the Supplement Myths”, you know that my wife and I did not change our diet overnight. Our diet evolved to something very close to the Planetary Diet over a period of years.
The Commission also purposely designed the Planetary Diet so that you “never have to say never” to your favorite foods. Three ounces of red meat a week does not sound like much, but it allows you a juicy steak once a month.
Sometimes you just need to develop a new mindset. As I shared in my books, my father prided himself on grilling the perfect steak. I love steaks, but I decided to set a few parameters. I don’t waste my red meat calories on anything besides filet mignon at a fine restaurant. It must be a special occasion, and someone else must be buying. That limits it to 2-3 times a year. I still get to enjoy good steak, and I stay well within the parameters of the Planetary diet.
Develop your strategy for enjoying some of your favorite foods within the parameters of the Planetary Diet and have fun with it.
The Bottom Line
Is your diet destroying the planet? This is not a new question, but a recent commission of international scientists has conducted a comprehensive study into our diet and its effect on our health and our environment. Their report serves as a dire warning of what will happen to us and our planet if we don’t change our ways.
The Commission carefully evaluated diet and food production methods and asked three questions:
- Are they good for us?
- Are they good for the planet?
- Are they sustainable? Will they be able to meet the needs of the projected population of 10 billion people in 2050 without degrading our environment.
The Commission described the typical American diet as a “lose-lose-lose diet”. It is bad for our health. It is bad for the planet. And it is not sustainable.
In its place they carefully designed their version of a primarily plant-based diet they called a “win-win-win diet”. It is good for our health. It is good for the planet. And, it is sustainable.
In their publication they refer to their diet as the “universal healthy reference diet” (What else would you expect from a committee?). However, it has become popularly known as the “Planetary Diet”.
The Planetary Diet is similar to other healthy diets such as semi-vegetarian, Mediterranean, DASH, and Flexitarian. However, what truly distinguishes it from the other diets is the restrictions placed on the non-plant portion of the diet to make it both environmentally friendly and sustainable (for details, read the article above).
I have spoken before about the importance of a primarily plant-based diet for our health. In that context it is a personal choice. It is optional.
However, this report is a wake-up call. It puts a primarily plant-based diet in an entirely different context. It is essential for the survival of our planet. It is no longer optional.
If you care about global warming…If you care about saving our planet, there is no other choice.
For more details read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.