The Role of Supplementation In Reducing Diabetes Risk
Author: Dr. Stephen Chaney
 Doctors usually discuss a holistic approach to diabetes with their patients. But, that often isn’t the case for other diseases. Why do doctors recommend drugs rather than natural approaches for controlling and treating other diseases? In part, it’s because so many Americans would rather take a pill than change their diet or lifestyle. Many of our doctors have become so conditioned to that expectation from their patients they don’t even suggest diet and lifestyle changes.
Doctors usually discuss a holistic approach to diabetes with their patients. But, that often isn’t the case for other diseases. Why do doctors recommend drugs rather than natural approaches for controlling and treating other diseases? In part, it’s because so many Americans would rather take a pill than change their diet or lifestyle. Many of our doctors have become so conditioned to that expectation from their patients they don’t even suggest diet and lifestyle changes.
That is our fault. We need to take responsibility for our health. Rather than just accepting whatever treatment our doctors suggest, we should partner with our doctors in designing the best treatment plan for us.
The other reason doctors often recommend drugs is that they are trained to base their decisions on evidence-based medicine. The Gold Standard for evidence-based medicine is, of course, a double blind, placebo controlled clinical trial. In those studies, a single component is compared to the placebo. That is easy to do when you are comparing a drug to a placebo. The drug either works better than the placebo, or it doesn’t.
Do Natural Remedies for Diabetes Work?
Of course, many of you are more interested in knowing whether holistic, natural approaches also work. That is a much more difficult question to answer.
Double blind, placebo controlled clinical studies are much more difficult to perform when you are looking at foods or nutrients. That’s because foods and nutrients are seldom effective by themselves. They interact with each other. It is the whole, rather than the individual components, that reduce the risk of diabetes and other diseases. Even worse, when you want to test the effectiveness of a holistic change in diet and lifestyle, how do you design a placebo?
 It reminds me of an international cancer symposium I attended over 30 years ago as a young Assistant Professor. A world-renowned cancer expert gave a talk from main stage and concluded by saying “I can show you, unequivocally, that colon cancer risk is significantly decreased by a lifestyle that includes a high-fiber diet, a low-fat diet, adequate calcium, adequate B vitamins, omega-3 fatty acids, exercise, and weight control. But, I can’t show you that any one of them, by themselves, is effective.”
It reminds me of an international cancer symposium I attended over 30 years ago as a young Assistant Professor. A world-renowned cancer expert gave a talk from main stage and concluded by saying “I can show you, unequivocally, that colon cancer risk is significantly decreased by a lifestyle that includes a high-fiber diet, a low-fat diet, adequate calcium, adequate B vitamins, omega-3 fatty acids, exercise, and weight control. But, I can’t show you that any one of them, by themselves, is effective.”
The question that came to me as I heard him speak was: “What’s the message that a responsible scientist or responsible health professional should be giving to their patients or the people that they are advising?” You’ve heard experts saying: “Don’t worry about the fat.” “Don’t worry about calcium.” “Don’t worry about B vitamins.” “Don’t worry about fiber.” “None of them can be shown to decrease the risk of colon cancer.”
Is that the message we should be giving people? Or should we really be saying what that doctor said many years ago – that a lifestyle that includes all those things significantly decreases the risk of colon cancer?
The problem is the negative studies you hear about, and your doctor hears about, are usually studies done with individual foods or individual nutrients. Those studies leave the impression that natural approaches don’t work. However, when you look at a holistic approach to diabetes, the answers are often much different.
Can a Holistic Approach to Diabetes Reduce Risk?
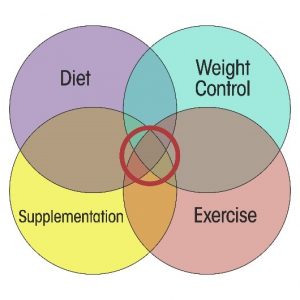 I created the diagram on the left for my book “Slaying the Food Myths” to represent holistic approaches to health. Simply put, diet, weight control, exercise, and supplementation all play a role in improving our health. It is that sweet spot in the middle of the diagram where we receive the optimal benefit. Finally, both diet and supplementation should also be holistic. No one food or nutrient will be effective by itself.
I created the diagram on the left for my book “Slaying the Food Myths” to represent holistic approaches to health. Simply put, diet, weight control, exercise, and supplementation all play a role in improving our health. It is that sweet spot in the middle of the diagram where we receive the optimal benefit. Finally, both diet and supplementation should also be holistic. No one food or nutrient will be effective by itself.
This is perfectly illustrated by a recent study (S.M. Kimball et al, Journal of Clinical & Translational Endocrinology, doi: 10.1016/j.jcte.2017.11.002 eCollection Dec 2017 ). If you just read the headlines, you would conclude the study was just about the effect of supplementation on the risk of developing diabetes. However, when you read the publication, you realized the study involves a lot more than supplementation.
The study was conducted by a non-profit wellness organization called Pure North S’Energy Foundation located in Calgary, Canada. They enrolled 188 middle-aged adults (ages 25-54 years) in the studies. Based on BMI measurements the participants were overweight, but not obese. They were followed for a two-year period.
Each of the participants met regularly with a health care professional who provided them with lifestyle advice. Specifically:
- They were advised to increase fruit and vegetable intake and reduce processed foods.
- If they had cardiovascular risk factors such as hypertension or hyperlipidemia, they were advised to go on the DASH diet.
- They were advised to follow an exercise routine that was appropriate for their health status.
In addition, the subjects were divided into two groups:
- Group 1 received a liquid vitamin D3 supplement consisting of 1,000 IU of vitamin D/drop. The dosage they received was individualized so that each subject received enough vitamin D to bring their blood levels of 25-hydroxy-vitamin D to an optimal level of >100 nmole/L.
- Group 2 received the vitamin D plus 600 mg of EPA and EPA, plus a very comprehensive multivitamin. In addition to the nutrients found in most multivitamins, their formulation contained carotenoids such as lutein and lycopene, polyphenols from wine grapes, N-acetyl cysteine, coenzyme Q10 and a host of other phytonutrients.
[Note: This supplement is not commercially available. However, I would not recommend it if it were. There appears to be little scientific rationale for the amounts of some ingredients.]
In short, all the subjects were put on a holistic diet and lifestyle program ( a holistic approach to diabetes ). Groupe 2 also received what I would consider a holistic supplement. Here were the results of the study.
- Neither group had significant weight loss or weight gain.
- Serum 25-hydroxyvitamin D increased significantly in both groups (the vitamin D supplementation was effective).
- HbA1c levels (a measure of blood sugar control) worsened slightly in Group 1 and improved slightly in Group 2.
However, those were average values. Individual subjects had much more significant changes in HbA1c. In fact, based on changes in HbA1c levels:
- 16% of Group 1 participants and only 8% of Group 2 participants progressed from normal blood sugar control to either prediabetes or diabetes.
- 8% of Group1 participants and 44% of Group 2 participants improved from prediabetes or diabetes to normal blood sugar control.
The authors of the study concluded: “The results suggest that nutrient supplementation may provide a safe, economical, and effective means for lowering diabetes risk. Further examination of this potential via randomized controlled trials is warranted.”
The Role of Supplementation In Reducing Diabetes Risk
 This is a single study and needs to be confirmed by future studies. However, if this study is confirmed, it has some interesting implications:
This is a single study and needs to be confirmed by future studies. However, if this study is confirmed, it has some interesting implications:
- It suggests a holistic approach to supplementation may be effective at decreasing diabetes risk.
- The holistic approach to supplementation was coupled with a holistic diet and lifestyle change in this study. We cannot assume that supplementation alone would have been effective in reducing diabetes risk.
- Since both Groups 1 and Group 2 included diet and lifestyle changes, we can conclude that the holistic diet and lifestyle changes in this study were not sufficient to reduce diabetes risk. Holistic supplementation was also required.
- The reason that diet and lifestyle changes did not affect diabetes risk in this study was most likely the failure to include a weight loss component. Multiple studies have shown that weight loss reduces diabetes risk.
The Bottom Line:
A recent study looked at the effect of a holistic diet, lifestyle and supplementation intervention on diabetes risk.
All participants in the study met regularly with a health care professional who provided them with lifestyle advice. Specifically:
- They were advised to increase fruit and vegetable intake and reduce processed foods.
- If they had cardiovascular risk factors such as hypertension or hyperlipidemia, they were advised to go on the DASH diet.
- They were advised to follow an exercise routine that was appropriate for their health status.
The subjects were divided into two groups:
- Group 1 received a liquid vitamin D3 supplement consisting of 1,000 IU of vitamin D.
- Group 2 received the vitamin D plus 600 mg of EPA and EPA, plus a very comprehensive multivitamin containing carotenoids such as lutein and lycopene, polyphenols from wine grapes, N-acetyl cysteine, coenzyme Q10 and a host of other phytonutrients.
Over a two-year period:
- 16% of Group 1 participants and only 8% of Group 2 progressed from normal blood sugar control to either prediabetes or diabetes.
- 8% of Group1 participants and 44% of Group 2 participants improved from prediabetes or diabetes to normal blood sugar control.
This is a single study and needs to be confirmed by future studies. However, if this study is confirmed, it has some interesting implications:
- It suggests a holistic approach to supplementation may be effective at decreasing diabetes risk.
- The holistic approach to supplementation was coupled with a holistic diet and lifestyle change in this study. We cannot assume that supplementation alone would have been effective in reducing diabetes risk.
- Since both Groups 1 and Group 2 included diet and lifestyle changes, we know that the holistic diet and lifestyle changes in this study were not sufficient to reduce diabetes risk. Holistic supplementation was also required.
- The reason that diet and lifestyle change did not affect diabetes risk was most likely the failure to include a weight loss component. Multiple studies have shown that weight loss reduces diabetes risk.
For more details, read the article above:
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
