Are Supplement Manufacturers Trying to Mislead You?
Author: Dr. Stephen Chaney
 There has been much confusion on folic acid vs. folate. For example, I recently received this question from a reader:
There has been much confusion on folic acid vs. folate. For example, I recently received this question from a reader:
“I have gotten so much clarification about folic acid from your video – thank you!
But I have another question I was hoping you could answer.When a supplement label states there is “folate” rather than “folic acid”, is there really a difference between the two? I hear women telling each other to only use the one that says folate because it’s made from food. And folic acid isn’t. These women are also paying more money for these products because of this. Is this true? (And I’m not talking about tetrahydrafolate, either)
I’ve been told by one manufacturer that they label it as folic acid, but they know other companies who use the exact same source of folic acid. Still, they put folate on their label, possibly to avoid controversy.
Are these women being duped? Should they be asking the manufacturer certain questions for clarification?”
The video, this reader is referring to is my “The Truth About Methyl Folate” video in which I debunk the many myths about methyl folate circulating on the internet, and, unfortunately, repeated by some doctors.
However, the reader is correct. I did not address the folic acid vs. folate nomenclature in that video. I will attempt to clarify it in this article.
Folic Acid vs. Folate
A Rose By Any Other Name
 I call this section “A Rose By Any Other Name” from the famous Shakespeare quote from Romeo and Juliet “A rose by any other names would smell as sweet”.
I call this section “A Rose By Any Other Name” from the famous Shakespeare quote from Romeo and Juliet “A rose by any other names would smell as sweet”.
Biochemists and nutritionists use the terms folic acid and folate interchangeably. There is a sound chemical rationale for that.
Folic acid has a glutamic acid residue on one end. Thus, folic acid is what chemists refer to as an organic acid, specifically a carboxylic acid. Under acidic conditions the appropriate suffix for an organic acid is “ic”. However, under neutral or alkaline conditions, organic acids lose their protons. Once that happens, the appropriate suffix is “ate”.
The exact pH of vitamin pills may vary from brand to brand. In our body our stomach is acidic, our intestines are alkaline, and our blood and cells are normally near neutral. Thus, vitamin B9 could correctly be labeled either folic acid or folate in supplements. It will be folic acid in our stomach and will be folate in our intestines, bloodstream, and cells. Beginning to see the difference between folic acid vs. folate?
The bottom line is that nobody is trying to trick you by using the term folate for the vitamin B9 on their supplement label. Furthermore, whether the label says folic acid or folate, the actual vitamin B9 will be in both the folic acid and folate form as it travels through your body.
In answer to your other question, since folic acid and folate are two names for the same molecule, folate is not more natural than folic acid. If someone is charging you extra because they use the term folate on their label, they are ripping you off.
What About Tetrahydrofolate?
 The person who sent me the question also asked about tetrahydrofolates. Here the story gets a bit murkier. As folic acid or folate enters our cells, three things immediately happen:
The person who sent me the question also asked about tetrahydrofolates. Here the story gets a bit murkier. As folic acid or folate enters our cells, three things immediately happen:
- It is reduced to tetrahydrofolate. That terminology simply means that 4 hydrogens have been added to the molecule.
- A string of glutamic acid residues is added. That traps it inside the cells.
- It is converted to a half dozen different derivatives that play important metabolic roles in the cell. N5-methyltetrahydrofolate (commonly referred to as methyl folate) is one of these metabolically active compounds.
This is where it gets confusing. Nutritionists also refer to all of these tetrahydrofolate derivatives as folates. My guess is that years ago some genius must have decided that the term tetrahydrofolate was too long and complicated for the general public.
In my view lumping everything together under the term folate has turned out to be more confusing in the long run. However, I do have the advantage of hindsight. It’s easy to point out mistakes after they are made.
However, this is where all of the confusion arises. It’s because the term folate can mean so many different things. Here are a few fast facts to help clarify the confusion.
- Folates in food are in the tetrahydrofolate form. Tetrahydrofolate in foods is, in fact, more natural than folic acid or folate in supplements. However, tetrahydrofolates in foods are utilized only about half as well as folic acid or folate in supplements. In addition, most of us don’t eat enough high-folate foods.
- In contrast, tetrahydrofolate in a supplement is not more natural than folic acid. That’s because:
- It would require one cup of lentils or two cups of spinach to provide the RDA level of tetrahydrofolate in a single vitamin tablet. That’s just one tablet. You do the math! If someone tells you that the folate in their supplement came from foods, they will lie to you about other things as well.
- In fact, the tetrahydrofolate found in supplements is chemically synthesized from folic acid. It can never be more natural than folic acid.
- Supplements containing tetrahydrofolate are no better utilized than supplements containing folic acid when you measure their ability to increase cellular tetrahydrofolate levels (the only measure that really matters).
The bottom line is that even if folate on the label were to refer to tetrahydrofolate, it is not from food. It is not more natural than folic acid. It is not better utilized than folic acid. If someone is charging you a higher price for that supplement, they are ripping you off.
Debunking The Methyl Folate Myths
 Methyl folate has become an internet sensation. If you believe all the hype, everyone should be using supplements containing methyl folate rather than folic acid. In fact, some of the claims made by manufacturers who sell methyl folate supplements are downright deceptive.
Methyl folate has become an internet sensation. If you believe all the hype, everyone should be using supplements containing methyl folate rather than folic acid. In fact, some of the claims made by manufacturers who sell methyl folate supplements are downright deceptive.
Unfortunately, there are even medical doctors touting the wonders of methyl folate and offering all sorts of plausible sounding biochemical explanations about why it is superior to folic acid. My take on that is that I try not to practice medicine when I write my articles. I have neither the training nor the degree to do that. In turn, I would ask medical doctors to stop trying to practice biochemistry.
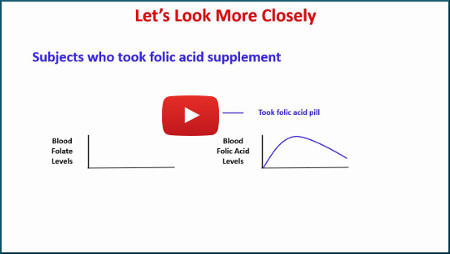
As I said at the beginning of this article, I have produced a video, “The Truth About Methyl Folate,” in which I debunk all the many methyl folate myths circulating on the internet. If you would like the “Cliff Notes” version, here it is:
- Supplements containing methyl folate do not get their methyl folate from foods.
- Methyl folate in supplements is chemically synthesized and is not more natural than folic acid.
- Folic acid and methyl folate in supplements are equally well utilized by the body, even in individuals with a MTHFR deficiency.
- Excess folic acid does not cause cancer.
If you would like the science and the references behind those statements, I invite you to view my video.
I hope you now understand folic acid vs. folates. If not, please feel free to reach out to me.
The Bottom Line
- A reader recently asked me to clear up the confusion about why the terms folic acid vs. folate are used interchangeably on supplement labels to describe vitamin B9.
- That terminology is based on simple chemistry. Folic acid and folate are two names for the same molecule. Under acidic conditions, it is called folic acid. Under neutral or alkaline conditions, it is called folate.
- Since folic acid and folate are two names for the same molecule, folate is not more natural than folic acid. If someone is charging you extra because they use the term folate on their label, they are ripping you off.
- In the cell folate is reduced to tetrahydrofolate and a number of metabolically active derivatives of tetrahydrofolate are formed. Unfortunately, these compounds are also referred to as folates. This terminology has a historical basis rather than a chemical basis and is confusing.
- If you see the term tetrahydrofolate on your supplement label, you need to know that it is not from food. It is not more natural than folic acid. It is not better utilized than folic acid. If someone is charging you a higher price for that supplement, they are also ripping you off.
- I have produced a video called “The Truth About Methyl Folate” to debunk the many methyl folate myths on the internet. In the article above, you will find the “Cliff Notes” version of the video.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.