Can A Healthy Lifestyle Improve Your Healthspan?
Author: Dr. Stephen Chaney
 Ever since Ponce de Leon led an expedition to the Florida coast in 1513, we have been searching for the mythical “Fountain Of Youth”. What does that myth mean?
Ever since Ponce de Leon led an expedition to the Florida coast in 1513, we have been searching for the mythical “Fountain Of Youth”. What does that myth mean?
Supposedly, just by immersing yourself in that fountain you would be made younger. You would experience all the exuberance and health you enjoyed when you were young. There have been many snake oil remedies over the years that have promised that. They were all frauds.
But what if you had it in your power to live longer and to retain your youthful health for most of those extra years. The ability to live healthier longer is something that scientists call “healthspan”. But you can think of it as your personal “Fountain Of Youth”.
Now comes the important question, “Can a healthy lifestyle improve your healthspan?” We know a healthy lifestyle is good for us. Most of us know what a healthy lifestyle is. But it’s so hard. Is it worth it? Will it actually increase our lifespan? Will it increase our healthspan?
Today I am sharing two studies from the prestigious Harvard T.H. Chan School of Public Health that answer those questions.
- The first study (Y Li et al, Circulation, 138: 345-355, 2018) looks at the effect of a healthy lifestyle on lifespan (how many years you can live).
- The second study (Y Li et al, British Medical Journal, 368: 16669, 2020) looks at the effect of a healthy lifestyle on healthspan (how many disease-free years you can live).
How Were The Studies Done?
 These studies started by combining the data from two major clinical trials:
These studies started by combining the data from two major clinical trials:
- The Nurse’s Health Study, which ran from 1980 to 2014.
- The Health Professional’s Follow-Up Study, which ran from 1986-2014.
These two clinical trials enrolled 78,865 women and 42,354 men and followed them for an average of 34 years. During this time there were 42,167 deaths. All the participants were free of heart disease, type 2 diabetes, and cancer at the time they were enrolled. Furthermore, the design of these clinical trials was extraordinary.
- A detailed food frequency questionnaire was administered every 2-4 years. This allowed the investigators to calculate cumulative averages of all dietary variables.
- Participants also filled out questionnaires that captured information on disease diagnosis every 2 years with follow-up rates >90%. This allowed the investigators to measure the onset of disease for each participant during the study. More importantly, 34 years is long enough to measure the onset of diseases like heart disease, diabetes, and cancer – diseases that require decades to develop.
-
- The questionnaires also captured information on medicines taken and lifestyle characteristics such as body weight, exercise, smoking and alcohol use.
- For analysis of diet quality, the investigators use something called the “Alternative Healthy Eating Index”. [The original Healthy Eating Index was developed about 10 years ago based on the 2010 “Dietary Guidelines for Americans”. Those guidelines have since been updated, and the “Alternative Healthy Eating Index” is based on the updated guidelines.] You can calculate your own Alternative Healthy Eating Index below, so you can see what is involved.
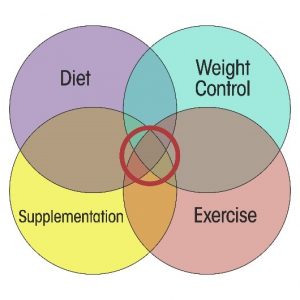
- Finally, the investigators included five lifestyle-related factors – diet, smoking, physical activity, alcohol consumption, and BMI (a measure of obesity) – in their estimation of a healthy lifestyle. Based on the best available evidence, they defined “low-risk” in each of these categories. Study participants were assigned 1 point for each low-risk category they achieved. Simply put, if they were low risk in all 5 categories, they received a score of 5. If they were low risk in none of the categories, they received a score of 0.
- Low risk for each of these categories was defined as follows:
-
- Low risk for a healthy diet was defined as those who scored in the top 40% in the Alternative Healthy Eating Index.
-
- Low risk for smoking was defined as never smoking.
-
- Low risk for physical activity was defined as 30 minutes/day of moderate or vigorous activities.
-
- Low risk for alcohol was defined as 0.5-1 drinks/day for women and 0.5-2 drinks/day for men.
-
- Low risk for weight was defined as a BMI in the healthy range (18.5-24.9 kg/m2).
Can A Healthy Lifestyle Improve Your Healthspan?
 The investigators compared participants who scored as low risk in all 5 categories with participants who scored as low risk in 0 categories (which would be typical for many Americans). For simplicity, I will refer to people who scored as low risk in 5 categories as having a “healthy lifestyle” and those who scored as low risk in 0 categories as having an “unhealthy lifestyle”.
The investigators compared participants who scored as low risk in all 5 categories with participants who scored as low risk in 0 categories (which would be typical for many Americans). For simplicity, I will refer to people who scored as low risk in 5 categories as having a “healthy lifestyle” and those who scored as low risk in 0 categories as having an “unhealthy lifestyle”.
The results of the first study were:
- Women who had had a healthy lifestyle lived 14 years longer than women with an unhealthy lifestyle (estimated life expectancy of 93 versus 79).
- Men who had a healthy lifestyle lived 12 years longer than men with an unhealthy lifestyle (estimated life expectancy was 87 versus 75).
- It was not necessary to achieve a perfect lifestyle. Life expectancy increased in a linear fashion for each low-risk lifestyle behavior achieved.
The authors of the study concluded: “Adopting a healthy lifestyle could substantially reduce premature mortality and prolong life expectancy in US adults. Our findings suggest that the gap in life expectancy between the US and other developed countries could be narrowed by improving lifestyle factors.”
The results of the second study were:
- Women who had a healthy lifestyle lived 11 years longer free of diabetes, heart disease, and cancer than women who had an unhealthy lifestyle (estimated disease-free life expectancy of 85 years versus 74 years).
- Men who had a healthy lifestyle lived 8 years longer free of diabetes, heart disease, and cancer than men who had an unhealthy lifestyle (estimated disease-free life expectancy of 81 years versus 73 years).
- Again, disease-free life expectancy increased in a linear fashion for each low-risk lifestyle behavior achieved.
The authors concluded: “Adherence to a healthy lifestyle at mid-life [They started their analysis at age 50] is associated with a longer life expectancy free of major chronic diseases. Our findings suggest that promotion of a healthy lifestyle would help reduce healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy.”
Can You Create Your Personal Fountain Of Youth?
 I posed the question at the beginning of this article, “Can you create your personal Fountain Of Youth”?” These two studies showed that you can improve both your life expectancy and your disease-free life expectancy by simply changing your lifestyle. So, the answer to the original question appears to be, “Yes, you can improve your healthspan. You can create your personal “Fountain of Youth.”
I posed the question at the beginning of this article, “Can you create your personal Fountain Of Youth”?” These two studies showed that you can improve both your life expectancy and your disease-free life expectancy by simply changing your lifestyle. So, the answer to the original question appears to be, “Yes, you can improve your healthspan. You can create your personal “Fountain of Youth.”
However, as a nation we appear to be moving in the wrong direction. The percentage of US adults adhering to a healthy lifestyle has decreased from 15% in 1988-1992 to 8% in 2001-2006.
Finally, I know you have some questions, and I have answers.
Question: What about supplementation? Will it also improve my healthspan?
Answer: When the investigators analyzed the data, they found that those with the healthiest lifestyles were also more likely to be taking a multivitamin. So, they attempted to statistically eliminate any effect of supplement use on the outcomes. That means these studies cannot answer that question.
However, if you calculate your Alternate Healthy Eating Index below, you will see that most of us fall short of perfection. Supplementation can fill in the gaps.
Question: I cannot imagine myself reaching perfection in all 5 lifestyle categories? Should I even try to achieve low risk in one or two categories?
Answer: The good news is that there was a linear increase in both life expectancy and disease-free life expectancy as people went from low-risk in one category to low-risk in all 5 categories. I would encourage you to try and achieve low risk status in as many categories as possible, but very few of us, including me, achieve perfection in all 5 categories.
Question: I am past 50 already. Is it too late for me to improve my healthspan?
Answer: Diet and some of the other lifestyle behaviors were remarkably constant over 34 years in both the Nurse’s Health Study and the Health Professional’s Follow-Up Study. That means that the lifespan and healthspan benefits reported in these studies probably resulted from adhering to a healthy lifestyle for most of their adult years.
However, it is never too late to start improving your lifestyle. You may not achieve the full benefits described in these studies, but you still can add years and disease-free years to your life.
How To Calculate Your Alternative Healthy Eating Index
You can calculate your own Alternative Healthy Eating Index score by simply adding up the points you score for each food category below.
Vegetables
Count 2 points for each serving you eat per day (up to 5 servings).
One serving = 1 cup green leafy vegetables or ½ cup for all other vegetables.
Do not count white potatoes or processed vegetables like French fries or kale chips.
Fruits
Count 2½ points for each serving you eat per day (up to 4 servings).
One serving = 1 piece of fruit or ½ cup of berries.
(do not count fruit juice or fruit incorporated into desserts or pastries).
Whole Grains
Count 2 points for each serving you eat per day (up to 5 servings).
One serving = ½ cup whole-grain rice, bulgur and other whole grains, cereal, and pasta or 1 slice of bread.
(For processed foods like pasta and bread, the label must say 100% whole grain).
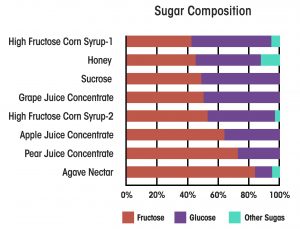
Sugary Drinks and Fruit Juice
Count 10 points if you drink 0 servings per week.
Count 5 points for 3-4 servings per week (½ serving per day).
Count 0 points for 7 or more servings per week (≥1 serving per day).
One serving = 8 oz. fruit juice, sugary soda, sweetened tea, coffee drink, energy drink, or sports drink.
Nuts and Beans
Count 10 points if you eat 7 or more servings per week (≥1 serving per day).
Count 5 points for 3-4 servings per week (½ serving per day).
Count 0 points for 0 servings per week.
One serving = 1 oz. nuts or seeds, 1 Tbs. peanut butter, ½ cup beans, 3½ oz. tofu.
Red and Processed Meat
Count 10 points if you eat 0 servings per week.
Count 7 points for 3-4 servings per week (½ serving per day).
Count 3 points for 3 servings per week (1 serving per day).
Count 0 points for ≥1½ servings per day.
One serving = 1½ oz. processed meats (bacon, ham, sausage, hot dogs, deli meat)
Or 4 oz. red meat (steak, hamburger, pork chops, lamb chops, etc.)
Seafood
Count 10 points if you eat 2 servings per week.
Count 5 points for 1 serving per week.
Count 0 points for 0 servings per week.
1 serving = 4 oz.
Now that you have your total, the scoring system is:
- 41 or higher is excellent
- 37-40 is good
- 33-36 is average (remember that it is average to be sick in this country)
- 28-32 is below average
- Below 28 is poor
Finally, for the purposes of these two studies, a score of 37 or higher was considered low risk.
The Bottom Line
Two recent studies have developed a healthy lifestyle score based on diet, exercise, body weight, smoking, and alcohol use. When they compared the effect of lifestyle on both lifespan (life expectancy) and healthspan (disease-free life expectancy), they reported:
- Women who had had a healthy lifestyle lived 14 years longer than women with an unhealthy lifestyle.
- Men who had a healthy lifestyle lived 12 years longer than men with an unhealthy lifestyle.
- Women who had a healthy lifestyle lived 11 years longer free of diabetes, heart disease, and cancer than women had an unhealthy lifestyle.
- Men who had a healthy lifestyle lived 8 years longer free of diabetes, heart disease, and cancer than men who had an unhealthy lifestyle.
- It is not necessary to achieve a perfect lifestyle. Lifespan and healthspan increased in a linear fashion for each low-risk lifestyle behavior (diet, exercise, body weight, smoking, and alcohol use) achieved.
- These studies did not evaluate whether supplement use also affects healthspan.
-
- However, if you calculate your diet with the Alternate Healthy Eating Index they used (see above), you will see that most of us fall short of perfection. Supplementation can fill in the gaps.
The authors concluded: “Our findings suggest that promotion of a healthy lifestyle would help reduce healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy.”
For more details, including how to calculate your Alternative Healthy Eating Index, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.