Where Do We Go From Here?
Author: Dr. Stephen Chaney
 Despite years of controversy, the benefits of omega-3s remain an active area of research. Over the next few weeks, I will review several groundbreaking omega-3 studies. This week I will focus on omega-3s and heart health.
Despite years of controversy, the benefits of omega-3s remain an active area of research. Over the next few weeks, I will review several groundbreaking omega-3 studies. This week I will focus on omega-3s and heart health.
I don’t need to tell you that the effect of omega-3s on heart health is controversial. One month a new study is published showing an amazing health benefit from omega-3 supplementation. A month or two later another study comes up empty. It finds no benefit from omega-3 supplementation.
That leads to confusion. On one hand you have websites and blogs claiming that omega-3s are a magic elixir that will cure all your ills. On the other hand, there are the naysayers, including many health professionals, claiming that omega-3 supplements are worthless.
I have discussed the reasons for the conflicting results from omega-3 clinical studies in previous issues of “Health Tips From the Professor”. You can go to https://chaneyhealth.com/healthtips/ and put omega-3s in the search box to read some of these articles.
Or if you prefer, I have also put together a digital download I call “The Omega-3 Pendulum” which briefly summarizes all my previous articles. It’s available on my Chaney Health School Teachable website.
Today I will discuss a study (B Bernhard et al, International Journal of Cardiology, 399; 131698, 2024) that asks whether 6 months of high dose omega-3 supplementation following a heart attack reduced the risk of major cardiovascular events over the next 6.6 years.
You might be wondering why the study didn’t just look at the effect of continuous omega-3 supplementation for 6 years following a heart attack. There are two very good reasons for the design of the current study.
1) The investigators wanted to do a double blind, placebo controlled clinical trial, the gold standard for clinical studies. However, that kind of study is impractical for a multi-year clinical trial. It would be prohibitively expensive, and patient compliance would be a big problem for a study that long.
2) The months immediately after a heart attack are critical in determining the long-term recovery of that patient. There is often a period of massive inflammation following a heart attack. And that can lead to further damage to the heart and reclosing of the arteries leading to the heart, both of which increase the risk of future adverse cardiac events.
Previous studies have shown that high dose omega-3s immediately following a heart attack can reduce inflammation and damage to the heart. However, those studies did not determine whether the cardioprotective effect of omega-3 supplementation immediately after a heart attack lead to improved long-term outcomes, something this study was designed to determine.
How Was The Study Done?
 The investigators enrolled 358 patients who had suffered a heart attack from three Boston area medical centers between June 2008 and August 2012.
The investigators enrolled 358 patients who had suffered a heart attack from three Boston area medical centers between June 2008 and August 2012.
The patient demographics were:
- Gender = 70% female.
- Average age = 59
- Average BMI = 29 (borderline obese).
- Patients with high blood pressure = 64%
- Patients with diabetes = 25%.
The patients were divided into two groups. The first group received capsules providing 4 gm/day of EPA, DHA, and other naturally occurring omega-3 fatty acids. The other group received a placebo containing corn oil. This was a double-blind study. Neither the patients nor the investigators knew which patients received the omega-3 fatty acids and which ones received the placebo.
The patients were instructed to take their assigned capsules daily for 6 months. At the beginning of the study, blood samples were withdrawn to determine the percentage of omega-3s in the fatty acid content of their red cell membranes (something called omega-3 index). Patients were also tested for insulin resistance and given a complete cardiovascular workup. This was repeated at the end of the 6-month study.
[Note: Previous studies have shown that an omega-3 index of 4% or lower is associated with high risk of heart disease, and an omega-3 index of 8% or above is associated with a low risk of heart disease.]
At 2-month intervals the patients were contacted by staff using a scripted interview to determine compliance with the protocol and their cardiovascular health. Once the 6 months of omega-3 supplementation was completed, the patients were followed for an additional 6.6 years. They were contacted every 6 months for the first 3 years and yearly between 3 years and 6 years.
The investigators quantified the number of major cardiac events (defined as recurrent heart attacks, the necessity for recurrent coronary artery bypass grafts, hospitalizations for heart failure, and all-cause deaths) for each patient during the 6.6-year follow-up period.
Patients in both groups were treated according to current “standard of care” protocols which consisted of diet and exercise advice and 5-6 drugs to reduce future cardiovascular events.
Do Omega-3s Improve Recovery From A Heart Attack?
 When the investigators looked at the incidence of adverse cardiac events during the 6.6-year follow-up period, there were three significant findings from this study.
When the investigators looked at the incidence of adverse cardiac events during the 6.6-year follow-up period, there were three significant findings from this study.
1) There were no adverse effects during the 6-month supplementation period with 4 gm/day of omega-3s. This is significant because a previous study with 4 gm/day of high purity EPA had reported some adverse effects which had led some critics to warn that omega-3 supplementation was dangerous. More study is needed, but my hypothesis is that this study did not have side effects because it used a mixture of all naturally occurring omega-3s rather than high purity EPA only.
However, this could also have been because of the way patients were screened before entering this study. I will discuss this in more detail below.
2) When the investigators simply compared the omega-3 group with the placebo group there was no difference in cardiovascular outcomes between the two groups. This may have been because this study faced significant “headwinds” that made it difficult show any benefit from supplementation. I call them “headwinds” rather than design flaws because they were unavoidable.
-
- It would be unethical to deny the standard of care to any patient who has just had a heart attack. That means that every patient in a study like this will be on multiple drugs that duplicate the beneficial effects of omega-3 fatty acids – including lowering blood pressure, lowering triglycerides, reducing inflammation, and reducing plaque buildup and blood clot formation in the coronary arteries.
That means that this study, and studies like it, cannot determine whether omega-3 fatty acids improve recovery from a heart attack. They can only ask whether omega-3 fatty acids have any additional benefit for patients on multiple drugs that duplicate many of the effects of omega-3 fatty acids. That significantly reduces the risk of a positive outcome.
-
- As I mentioned above, it would have been impractical to continue providing omega-3 supplements and placebos during the 6.6-year follow-up.
And the study was blinded, meaning that the investigators did not know which patients got the omega-3s and which patients got the placebo. That meant the investigators could not advise the omega-3 supplement users to continue omega-3 supplementation during the follow-up period.
Consequently, the study could only ask if 6 months of high-dose omega-3 supplementation had a measurable benefit 6.6 years later. I, for one, would be more interested in knowing whether lower dose omega-3 supplementation continued for the duration of this study reduced the risk of major coronary events.
3) When the investigators compared patients who achieved a significant increase in their omega-3 index during the 6-month supplementation period with those who didn’t, they found a significant benefit of omega-3 supplementation.
This was perhaps the most significant finding from this study.
If the investigators had stopped by simply comparing omega-3 users to the placebo, this would have been just another negative study. We would be wondering why it did not show any benefit of omega-3 fatty acid supplementation.
However, these investigators were experts on the omega-3 index. They knew that there was considerable individual variability in the efficiency of omega-3 uptake and incorporation into cell membranes. In short, they knew that not everyone taking a particular dose of omega-3s will achieve the same omega-3 index.
And that is exactly what they saw in this study. All the patients in the 6-month omega-3 group experienced an increase in omega-3 index, but there was considerable variability in how much the omega-3 index increased over 6 months.
So, the investigators divided the omega-3 group into two subgroups – ones whose omega-3 index increased by ≥ 5 percentage points (sufficient to move those patients from high risk of heart disease to low risk) and ones whose omega-3 index increased by less than 5 percentage points.
When the investigators compared patients with ≥ 5% increase in omega-3 index to those with <5% increase in omega-3 index:
- Those with an increase in omega-3 index of ≥ 5% had a 2.9% annual risk of suffering major adverse cardiac events compared to a 7.1% annual risk for those with an increase of <5%.
- That’s a risk reduction of almost 60%, and it was highly significant.
The authors concluded, “In a long-term follow-up study, treatment with [high dose] omega-3s for 6 months following a heart attack did not reduce adverse cardiac events compared to placebo. However, those patients who were treated with omega-3s and achieved ≥ 5% rise in omega-3 index experienced a significant reduction of adverse cardiac events after a median follow-up period of 6.6 years…Additional studies are needed to confirm this association and may help identify who may benefit from omega-3 fatty acid treatment following a heart attack.”
What Does This Study Mean For You?
 I should start by saying that I do not recommend 4 gm/day of omega-3 fatty acids following a heart attack without checking with your doctor first.
I should start by saying that I do not recommend 4 gm/day of omega-3 fatty acids following a heart attack without checking with your doctor first.
- If you are on a blood thinning medication, the dose of either the medication or the omega-3 supplement may need to be reduced to prevent complications due to excess bleeding.
- In addition, the investigators excluded patients from this study who might suffer adverse effects from omega-3 supplementation. This is a judgement only your doctor can make.
With that advice out of the way, the most important takeaway from this study is that uptake and utilization of omega-3 fatty acids varies from individual to individual.
The omega-3 index is a measure of how well any individual absorbs and utilizes dietary omega-3s. And this study shows that the omega-3 index is a much better predictor of heart health outcomes than the amount of omega-3 fatty acids a person consumes.
This is not surprising because multiple studies have shown that the omega-3 index correlates with heart health outcomes. It may also explain why many studies based on omega-3 intake only have failed to show a benefit of omega-3 supplementation.
Vitamin D supplementation is a similar story. There is also considerable variability in the uptake of vitamin D and conversion to its active form in the body. 25-hydroxy vitamin D levels in the blood are a marker for active vitamin D. For that reason, I have long recommended that you get your 25-hydroxy vitamin D level tested with your annual physical and, with your doctor’s help, base the dose of the vitamin D supplement you use on that test.
This study suggests that we may also want to request an omega-3 index test and use it to determine the amount of supplemental omega-3s we add to our diet.
Where Do We Go From Here?
 The idea that we need to use the omega-3 index to determine the effectiveness of the omega-3 supplement we use is novel. As the authors suggest, we need more studies to confirm this effect. There are already many studies showing a correlation of omega-3 index with heart health outcomes. But we need more double blind, placebo-controlled studies like this one.
The idea that we need to use the omega-3 index to determine the effectiveness of the omega-3 supplement we use is novel. As the authors suggest, we need more studies to confirm this effect. There are already many studies showing a correlation of omega-3 index with heart health outcomes. But we need more double blind, placebo-controlled studies like this one.
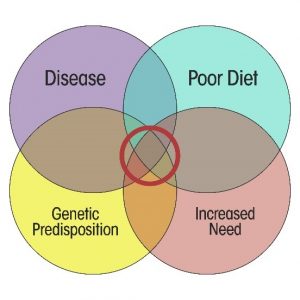
More importantly, we need to understand what determines the efficiency of supplemental fatty acid utilization so we can predict and possibly improve omega-3 utilization. The authors suggested that certain genetic variants might affect the efficiency of omega-3 utilization. But the variability of omega-3 utilization could also be affected by:
- Diet, especially the presence of other fats in the diet.
- Metabolic differences due to obesity and diseases like diabetes.
- Gender, ethnicity, and age.
- Design of the omega-3 supplement.
We need much more research in these areas, so we can personalize and optimize omega-3 supplementation on an individual basis.
The Bottom Line
A recent study asked whether high dose omega-3 supplementation for 6 months following a heart attack reduced major cardiac events during the next 6.6 years.
- When they simply compared omega-3 supplementation with the placebo there was no effect of omega-3 supplementation on cardiac outcomes.
- However, when they based their comparison on the omega-3 index (a measure of how efficiently the omega-3s were absorbed and incorporated into cell membranes), the group with the highest omega-3 index experienced a 60% reduction in adverse cardiac events over the next 6.6 years.
This is consistent with multiple studies showing that the omega-3 index correlates with heart health outcomes.
More importantly, this study shows there is significant individual variation in the efficiency of omega-3 absorption and utilization. It also suggests that recommendations for omega-3 supplementation should be based on the omega-3 index achieved rather than the dose or form of the omega-3 supplement.
For more information on this study and what it means for you read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.