Will Fish Oil Lower Your Blood Pressure?
Author: Dr. Stephen Chaney
 Is there a relationship between omega-3 and blood pressure we should understand to for health benefits?
Is there a relationship between omega-3 and blood pressure we should understand to for health benefits?
High blood pressure is a killer! It can kill you by causing heart attacks, strokes, congestive heart failure, kidney failure and much more.
High blood pressure is a serial killer. It doesn’t just kill a few people. It kills lots of people. The American Heart Association estimates that high blood pressure directly or indirectly caused 363,000 deaths in 2010. That is almost 1 person every second and represents a 41% increase from 2000. It’s because high blood pressure is not a rare disease.
- 31% of Americans have high blood pressure, also called hypertension, (defined as a systolic blood pressure of 140 mm Hg or more or a diastolic blood pressure of 90 mm Hg or more).
- Another 30% of Americans have prehypertension (systolic blood pressure of 120-139 mm Hg or diastolic blood pressure of 80-89 mm Hg).
That’s over 61% of Americans with abnormal blood pressure!
High blood pressure is a silent killer. That’s because it is a very insidious disease that sneaks up on you when you least expect it. Systolic blood pressure increases 0.6 mm Hg/year for most adults over 50. By age 75 or above 76-80% of American adults will have high blood pressure. Even worse, many people with high blood pressure have no symptoms, so they don’t even know that their blood pressure is elevated. For them the first symptom of high blood pressure is often sudden death.
Blood pressure medications can harm your quality of life. Blood pressure medications save lives. However, like most drugs, blood pressure medications have a plethora of side effects – including weakness, dizziness, fainting, shortness of breath, chest pain, nausea, diarrhea or constipation, heartburn, depression, heart palpitations, and even memory loss . The many side effects associated with blood pressure medications lead to poor compliance, which is probably why only 47% of patients with high blood pressure are adequately controlled.
You do have natural options. By now you are probably wondering whether there are natural approaches for controlling your blood pressure that are both effective and lack side effects. The answer is a resounding YES! I’ll outline a holistic natural approach for keeping your blood pressure under control in a minute, but let me start with the good news about omega-3 fatty acids.
The Good News About Omega-3 and Blood Pressure
 What’s the good news about omega-3 and blood pressure? We’ve known for some time that omega-3 fatty acids helped lower blood pressure, but two recent studies have really highlighted just how strong the effect of omega-3s on lowering blood pressure is.
What’s the good news about omega-3 and blood pressure? We’ve known for some time that omega-3 fatty acids helped lower blood pressure, but two recent studies have really highlighted just how strong the effect of omega-3s on lowering blood pressure is.
The first study (Miller et al, American Journal of Hypertension, 27: 885-896, 2014) was a meta-analysis of 70 randomized, placebo-controlled clinical trials of long chain omega-3 (EPA + DHA) supplementation and blood pressure.
Here are the results of this study:
- In the group with normal blood pressure at the beginning of the study EPA + DHA supplementation decreased systolic blood pressure by 1.25 mm Hg.
- Given that systolic blood pressure rises an average of 0.6 mm Hg/year in adults over 50, the authors estimated that omega-3 supplementation alone would delay the onset of age-related high blood pressure by 2 years.
- In the group with elevated blood pressure not taking medication at the beginning of the study, EPA + DHA supplementation decreased systolic blood pressure by an impressive 4.51 mm Hg and diastolic blood pressure by 3.05 mm Hg.
- The authors noted that this decrease in systolic blood pressure could “prevent an individual from requiring medication [with all its side effects] to control their hypertension” or decrease the amount of medication required.
However, the doses of omega-3s used in these studies ranged from 1 to over 4 grams/day (mean dose = 3.8 grams/day). That sparked a second study (Minihane et al, Journal of Nutrition, 146: 516-523, 2016) to see whether lower levels of omega-3s might be equally effective. This study was an 8 week double-blind, placebo-controlled study comparing the effects of 0.7 or 1.8 grams of EPA + DHA per day (versus an 8:2 ratio of palm and soybean oil as a placebo) on blood pressure.
Here are the results of this study:
- In the group with normal blood pressure at the beginning of the study, EPA + DHA supplementation caused no significant decrease in blood pressure. This could be due to the smaller number of subjects or the lower doses of EPA + DHA used in this study.
- In the group with elevated blood pressure not taking medication at the beginning of the study, EPA + DHA supplementation decreased systolic blood pressure by 5 mm Hg and, the effect was essentially identical at 0.7 grams/day and 1.8 grams/day.
- The authors concluded “Our data suggest that increased EPA + DHA intakes of only 0.7 grams/day may be an effective strategy for blood pressure control.”
A Holistic Approach To Blood Pressure Control
 The latest information about omega-3 and blood pressure is good news indeed, but that’s not the only natural approach that lowers blood pressure. You have lots of other arrows in your quiver. For example:
The latest information about omega-3 and blood pressure is good news indeed, but that’s not the only natural approach that lowers blood pressure. You have lots of other arrows in your quiver. For example:
- The DASH diet (A diet that has lots of fresh fruits and vegetables; includes whole grains, low fat dairy, poultry, fish, beans, nuts and oils; and is low in sugar and red meats) reduces systolic blood pressure by 5-6 mm Hg. [Low sodium, low sodium/high-potassium, low-sodium/low-calorie, low-calorie and Mediterranean diets also lower blood pressure, but not by as much as the DASH diet].
- Reducing sodium by about 1,150 mg/day reduces systolic blood pressure by 3-4 mm Hg.
- Reducing excess weight by 5% reduces systolic blood pressure by 3 points.
- Doing at least 40 minutes of aerobic exercise 3-4 times/week reduces systolic blood pressure by 2-5 mm Hg.
- Nitrates, whether derived from fresh fruits and vegetables or from supplements probably also reduce blood pressure , but we don’t yet know by how much.
 If you’ve been keeping track, you’ve probably figured out that a holistic lifestyle that included at least 0.7 grams/day of long chain omega-3s (EPA + DHA) plus everything else in the list above could reduce your systolic blood pressure by a whopping 18-22 mm Hg.
If you’ve been keeping track, you’ve probably figured out that a holistic lifestyle that included at least 0.7 grams/day of long chain omega-3s (EPA + DHA) plus everything else in the list above could reduce your systolic blood pressure by a whopping 18-22 mm Hg.
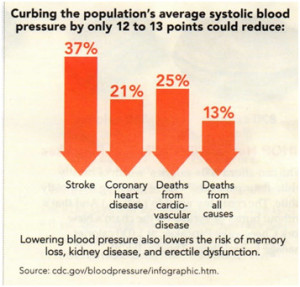
That’s significant because,as the graphic on the right shows, the CDC estimates that reducing high systolic blood pressure by only 12-13 mm Hg could substantially decrease your risk of disease.
A Word Of Caution
While holistic approaches have the potential to keep your blood pressure under control without the side effects of medications, it is important not to blindly rely on holistic approaches alone. There are also genetic and environmental risk factors involved in determining blood pressure. You could be doing everything right and still have high blood pressure. Plus, you need to remember that high blood pressure is a silent killer that often doesn’t have any detectable symptoms prior to that first heart attack or stroke.
My recommendations are:
- Monitor your blood pressure on a regular basis.
- If your blood pressure starts to become elevated, consult with your doctor about starting with natural approaches to bring your blood pressure back under control. Doctors are fully aware of the side effects of blood pressure medications, and most doctors are happy to encourage you to try natural approaches first.
- Continue to monitor blood pressure as directed by your doctor. If natural approaches are insufficient to bring your blood pressure under control, they will prescribe the lowest dose of blood pressure medication possible to get your blood pressure where it needs to be.
- Don’t stop making holistic lifestyle choices to reduce blood pressure just because you are on medication. The more you do to keep your blood pressure under control, the less medication your doctor will need to use (That means fewer side effects).
The Bottom Line
- Recent studies have shown that supplementation with as little as 0.7 grams of long chain omega-3s (EPA + DHA) per day is sufficient to decrease systolic blood pressure by ~ 5 mm Hg in people with untreated hypertension (high blood pressure). If your blood pressure is currently in the normal range, it is not yet clear how much EPA + DHA you need to keep it there. That may require a higher dose.
- When you combine that with other natural approaches such as the DASH diet, reducing sodium, losing weight, and increasing exercise you can decrease blood pressure by 18-22 mm Hg.
- The CDC estimates that is enough to substantially decrease your risk of stroke, coronary heart disease, memory loss, kidney disease, erectile dysfunction, death from cardiovascular disease, and death from any cause.
- The authors of these recent studies concluded that holistic lifestyle changes including substantially increasing omega-3 intake have the potential to significantly delay the onset of age-related hypertension and may allow people with elevated blood pressure to eliminate or substantially reduce the use of blood pressure medications – with their many side effects.
- High blood pressure is a silent killer. It is important to monitor your blood pressure regularly. If it becomes elevated, work with your doctor to find the balance of natural approaches and medication that is right for you.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
