Clearing Up The Calcium Confusion
Author: Dr. Stephen Chaney
 Should we take calcium supplements? You have every right to be confused about calcium supplementation. There have been a lot of conflicting headlines in recent months.
Should we take calcium supplements? You have every right to be confused about calcium supplementation. There have been a lot of conflicting headlines in recent months.
It has seemed like a no-brainer for years that calcium supplementation could help post-menopausal women and men over 50 avoid the debilitating effects of osteoporosis.
After all:
- >99% of adults fail to get the USDA recommended 2.5-3 servings/day of dairy products.
- 67% of women ages 19-50 and 90% of women over 50 fail to meet the RDA recommendations for calcium intake from diet alone.
- Men do a little better (but only because we consume more food). 40% of men ages 19-50 and 80% of men over 50 fail to meet the RDA recommendations for calcium intake from diet alone.
- Inadequate calcium intake over a lifetime is considered a major risk factor for osteoporosis.
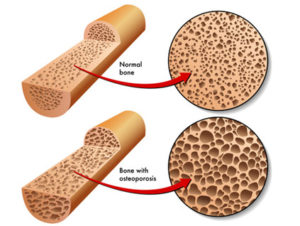
- Osteoporosis is serious business. It doesn’t just cause bone fractures. It can result in chronic pain, disability, long term nursing home care, and even death.
It’s no wonder that some experts have predicted that supplementation with calcium and vitamin D could save over $1 billion per year in health care cost savings. It is also why health professionals have recommended calcium supplementation for years, especially for postmenopausal women and men over 50.
However, recent headlines have claimed that calcium supplementation doesn’t really increase bone density or prevent osteoporosis (more about that later). Other headlines have suggested that calcium supplementation is actually bad for you. It may increase your risk of heart disease.
That’s why the general public, and even many doctors, are confused. Should we take calcium supplements? Everyone wants to know the answer to two questions:
- Do calcium supplements work?
- Are calcium supplements safe?
I will start with the second question first.
Are Calcium Supplements Safe?
 I have discussed the issue of calcium supplements and heart disease risk in a previous issue of Health Tips From the Professor. Briefly, the initial studies suggesting that calcium supplementation might increase the risk of heart attacks and cardiovascular disease were good studies, but they were small, short-term studies.
I have discussed the issue of calcium supplements and heart disease risk in a previous issue of Health Tips From the Professor. Briefly, the initial studies suggesting that calcium supplementation might increase the risk of heart attacks and cardiovascular disease were good studies, but they were small, short-term studies.
The initial studies raised an important question, so the scientific community stepped up to the plate and conducted larger, longer term studies to test the hypothesis. Both of those studies concluded that calcium supplementation posed no heart health risks.
Now a third major study on the subject has just been published (Raffield et al, Nutrition, Metabolism & Cardiovascular Disease, doi: 10.1016/j.numecd.2016.07.007). The study followed 6236 men and women ages 45-84 for an average of 10.3 years. The subjects were from four different race/ethnicity groups and came from 6 different locations in the United States. More importantly, there were 208 heart attacks and 641 diagnoses of cardiovascular disease during the study, so the sample size was large enough to accurately determine the relationship between calcium supplementation and heart disease.
The results were pretty straight forward:
- The authors concluded: “[This study] does not support a substantial association of calcium supplement use with negative cardiovascular outcomes.” If you would like the plain-speak version of their conclusion, they were saying that they saw no increase in either heart attacks or overall cardiovascular disease in people taking calcium supplements.
- If anything, they saw a slight decrease in heart attack risk in those taking calcium supplements, but this was not statistically significant.
In summary, the weight of evidence is pretty clear. Three major studies have now come to the same conclusion: Calcium supplementation does not increase the risk of either heart attacks or cardiovascular disease.
Of course, once information has been placed on the internet, it tends to stay there for a very long time – even if subsequent studies have proven it to be wrong. So the myth that calcium supplementation increases heart attack risk will probably be with us for a while.
So, should we take calcium supplements? Let’s first investigate a little further.
Do Calcium Supplements Work?
 As I mention above, recent headlines have also suggested that calcium supplementation does not increase bone density, so it is unlikely to protect against osteoporosis. I analyzed the study behind those headlines in great detail in two previous issues of Health Tips From the Professor.
As I mention above, recent headlines have also suggested that calcium supplementation does not increase bone density, so it is unlikely to protect against osteoporosis. I analyzed the study behind those headlines in great detail in two previous issues of Health Tips From the Professor.
In Part 1 Calcium Supplements Prevent Bone Fractures I pointed out the multiple weaknesses in the study that make it impossible to draw a meaningful conclusion from the data.
In Part 2 Preventing Osteoporosis I discussed the conclusion that the study should have come to, namely: Adequate calcium intake is absolutely essential for strong bones, but calcium intake is only one component of a bone healthy lifestyle.
The bottom line is that calcium supplementation will be of little use if:
- You aren’t getting adequate amounts of vitamin D and all of the other nutrients needed for bone formation from diet and supplementation.
- You aren’t getting enough exercise to stimulate bone formation.
- You are consuming bone dissolving foods or taking bone dissolving drugs.
Conversely, none of the other aspects of a bone healthy lifestyle matter if you aren’t getting enough calcium from diet and supplementation.
The bottom line is that you need to get adequate calcium and have a bone healthy lifestyle to build strong bones and prevent osteoporosis, and calcium supplementation is often essential to make sure you are getting adequate calcium.
Should We Take Calcium Supplements?
 Should we take calcium supplements? If you are one of the millions of Americans who aren’t meeting the RDA guidelines for calcium from diet alone, the answer is an unqualified yes. Calcium supplementation is safe, and it is cheap. Osteoporosis is preventable, and it is not a disease to be trifled with.
Should we take calcium supplements? If you are one of the millions of Americans who aren’t meeting the RDA guidelines for calcium from diet alone, the answer is an unqualified yes. Calcium supplementation is safe, and it is cheap. Osteoporosis is preventable, and it is not a disease to be trifled with.
However, you also need to be aware that calcium supplementation alone is unlikely to be effective unless you follow a bone healthy lifestyle of diet, exercise and appropriate supplementation to make sure you are getting all of the nutrients needed for bone formation.
Of course, it is always possible to get too much of a good thing. The RDA for calcium is 1,000 – 1,200 mg/day. The suggested upper limit (UL) for calcium is 2,000 – 3,000 mg/day. I would aim closer to the RDA than the UL unless higher intakes are recommended by your health care professional.
The Bottom Line
- 80% of men and 90% percent of women over 50 do not get enough calcium from their diet.
- Consequently, doctors have consistently recommended calcium supplementation to prevent osteoporosis, and 50% of men and 60% of women over 60 currently consume calcium supplements on a regular basis.
- Some small, short term studies suggested that calcium supplementation might increase the risk of heart disease, and warnings about calcium supplementation have been widely circulated on the internet. This hypothesis has been evaluated by three larger, longer term studies that have all concluded that calcium supplementation does not increase heart disease risk.
- A recent study claimed that calcium supplementation was ineffective at increasing bone density, and that report has also been widely circulated. However, there are multiple weaknesses in the study that make it impossible to draw a meaningful conclusion from the data.
- If you are one of the millions of Americans who aren’t meeting the RDA guidelines for calcium from diet alone, you should consider calcium supplementation. It is safe. It is effective when combined with a bone healthy lifestyle of diet, exercise, and appropriate supplementation. Finally, it is cheap. Osteoporosis is preventable, and it is not a disease to be trifled with.
- Of course, it is always possible to get too much of a good thing. The RDA for calcium is 1,000 – 1,200 mg/day. The suggested upper limit (UL) for calcium is 2,000 – 3,000 mg/day. I would aim closer to the RDA than the UL unless higher intakes are recommended by your health care professional.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
