The Dark Side Of Hormone Replacement Therapy
Author: Dr. Stephen Chaney
 When I was still teaching, a physician and I were co-directors of one of the first courses medical students took at UNC. In his opening lecture to these brand-new medical students, one of his pearls of wisdom was the statement, “The only safe drug is a new drug.”
When I was still teaching, a physician and I were co-directors of one of the first courses medical students took at UNC. In his opening lecture to these brand-new medical students, one of his pearls of wisdom was the statement, “The only safe drug is a new drug.”
After a pause to let the students think about it, he followed up with, “That’s because the side effects haven’t been discovered yet.”
He would then go on to explain that every drug must go through rigorous clinical trials, and some side effects are discovered then. But some of the most serious side effects aren’t discovered until years later after 100’s of thousands of patients had used the drugs.
Hormone replacement therapy is a perfect example of this principle. Hormone replacement therapy was first introduced in the 1960s. At first it seemed to be an almost miraculous solution to menopausal symptoms.
Millions of women were overjoyed. After all, menopause symptoms can make life miserable. They include:
- Hot flashes
- Night sweats
- Sleep disturbances
- Mood swings
- Depression
- Anxiety
- Forgetfulness
- Food cravings
- Tiredness
Just to name a few. While only 25% of women experience severe symptoms, why would anyone want to experience any of these symptoms?
And doctors were only too happy to oblige. Why not? The known side effects were mild. Why should any woman experience menopause symptoms?
But that was before the dark side of hormone replacement therapy started to emerge.
The Dark Side Of Hormone Replacement Therapy
 The popularity of hormone replacement therapy peaked in the 1990s. It was around that time that reports started to emerge suggesting that hormone replacement therapy increased the risk of heart disease and breast cancer. Those risks were confirmed in a major study called the Woman’s Health Initiative that was published in 2002.
The popularity of hormone replacement therapy peaked in the 1990s. It was around that time that reports started to emerge suggesting that hormone replacement therapy increased the risk of heart disease and breast cancer. Those risks were confirmed in a major study called the Woman’s Health Initiative that was published in 2002.
That study caused a major shift in how the medical community regarded hormone replacement therapy. Within a few years doctors shifted from recommending hormone replacement therapy for every woman with menopausal symptoms to recommending it only in cases where the symptoms were debilitating and only for the shortest possible time.
The effect on women’s health was huge. In fact, switching from universal hormone replacement therapy to targeted hormone replacement therapy remains the single most effective public health measure for reducing the incidence of breast cancer. It is more effective than any of new drugs and measures to improve breast cancer screening since then.
I wish I could tell you that was the end of the story. But recent studies have suggested that hormone replacement therapy also increases the risk of dementia. Unfortunately, most of those studies have had flaws, so the link between hormone replacement therapy and dementia has remained controversial – until now.
The study (N Pourhadi et al, British Medical Journal, 382, e072770, 2023) I will describe today was designed to provide a more definitive test of this hypothesis.
How Was This Study Done?
 This was done in Denmark and used the Danish health registries. As Americans, you might not be aware of what a rich resource those health registries are. One advantage of socialized medicine is that every aspect of your health is tracked and recorded from cradle to grave.
This was done in Denmark and used the Danish health registries. As Americans, you might not be aware of what a rich resource those health registries are. One advantage of socialized medicine is that every aspect of your health is tracked and recorded from cradle to grave.
[I’m not sure I would be comfortable with our government knowing that much about me, but it is a treasure-trove of information if you want to conduct a study like this one.]
The authors used the Danish National Health registries to:
- Identify all Danish women aged 50-60 who had no incidence of dementia and were not on hormone replacement therapy as of January 1, 2000.
- Identify 5589 women (1.8% of the population) from this group who were diagnosed with dementia between January 1, 2000 and December 31, 2018 and match them with 55,890 controls who remained dementia-free through the end of 2018.
- Using the National Prescription registry, they were able to track which women used hormone-replacement therapy, what kind of therapy it was (there are several variations of hormone replacement therapy), and how long they remained on hormone replacement therapy.
The average age at which hormone replacement therapy began was 53, and the average duration of use was 3.8 years. The average age of a dementia diagnosis was 70.
Does Hormone Replacement Therapy Cause Dementia?
 When the authors compared women who used an estrogen-progestin combination hormone replacement therapy (the most common kind) with women who never used hormone replacement therapy, the hormone replacement therapy users were:
When the authors compared women who used an estrogen-progestin combination hormone replacement therapy (the most common kind) with women who never used hormone replacement therapy, the hormone replacement therapy users were:
- 24% more likely to develop dementia of any kind.
- 21% more likely to develop late-onset dementia.
- 22% more likely to develop Alzheimer’s disease.
Longer duration of hormone replacement use was associated with an increased risk of dementia. The increased risk of dementia was:
- 21% for ≤ 1 year duration.
- 39% for 8-12 years duration.
- 74% for > 12 years duration.
The age at which hormone replacement therapy was begun had a slight effect on dementia risk. The increased risk of dementia was:
- 26% when it was started at age 45-50.
- 21% when it was started at age 51-60.
Finally, other forms of hormone replacement therapy such as progestin only therapy and vaginal estrogen treatment did not have a statistically significant effect on dementia risk. But it was not clear whether this was due to a smaller sample size or whether it was a true null effect.
The authors concluded, “Menopausal hormone replacement therapy was positively associated with the development of all cause dementia and Alzheimer’s disease, even in women who received treatment at the age of 55 years or younger.”
The Pros And Cons Of This Study
 The pros are obvious. This was a large, well-designed study. And its use of the Danish National Health registry and National Prescription registry allowed it to address the dementia risk of hormone replacement therapy in a comprehensive manner.
The pros are obvious. This was a large, well-designed study. And its use of the Danish National Health registry and National Prescription registry allowed it to address the dementia risk of hormone replacement therapy in a comprehensive manner.
The cons are also obvious. This was an observational study. It can only show associations, not prove cause and effect. [I should note that it would be impossible to do a double-blind study to prove cause and effect. The size of the population group and the length of time required would make that kind of study unworkable.]
As I have said in previous issues of “Health Tips From the Professor”, the Achilles heel of observational studies is the possibility that a confounding variable (something else about the women who developed dementia) was the true cause of the observed outcome (in this case, increased dementia risk).
The authors did an excellent job of identifying known confounding variables that might have contributed to dementia and statistically correcting for them. However, the authors identified one potential confounding variable I would not have thought of.
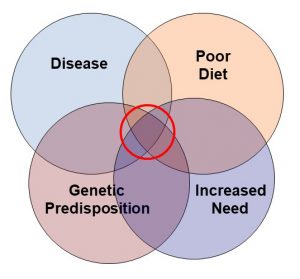
In the words of the authors, “Further studies are warranted to determine whether these findings represent an actual effect of menopausal hormone therapy on dementia risk, or whether they reflect an underlying predisposition in women in need of these treatments.”
In case you need a translation, the authors are saying that it is possible that certain women have an underlying disease state or genetic predisposition that makes them very sensitive to menopausal symptoms (which increases the likelihood that they would receive hormone replacement therapy to reduce their symptoms) and increases their risk of dementia. In that case, it would be the underlying medical condition or genetic predisposition that was responsible for the increased dementia risk, not the hormone replacement therapy.”
I consider that unlikely, but it does warrant future studies.
Is Hormone Replacement Therapy Right For You?
 Ultimately, this is your decision. But this is a decision you should make with your health care provider.
Ultimately, this is your decision. But this is a decision you should make with your health care provider.
It is clear that hormone replacement therapy increases your risk of heart disease, breast cancer, and may increase your risk of dementia.
In part, your decision depends on the severity of your symptoms and your willingness to accept the risks associated with alleviating those symptoms.
But your health care provider can also help you consider family history and unrelated health conditions that may also increase your risk of these diseases. If your underlying disease risk is low, would you be more willing or less willing to accept the risks associated with hormone replacement therapy? Again, this is your decision.
And, if you decide to proceed with hormone replacement therapy, your health care provider can recommend the type of therapy and length of therapy that will minimize your risks.
The Bottom Line
Several recent studies have suggested that hormone replacement therapy may increase the risk of dementia, but this has remained controversial.
In this issue of “Health Tips From the Professor” I share a very large, well designed study that supports the link between hormone replacement therapy and dementia.
When the authors of this study compared women who had used hormone replacement therapy with women who never used hormone replacement therapy, the hormone replacement therapy users were:
- 24% more likely to develop dementia of any kind.
- 21% more likely to develop late-onset dementia.
- 22% more likely to develop Alzheimer’s disease.
The authors concluded, “Menopausal hormone replacement therapy was positively associated with the development of all cause dementia and Alzheimer’s disease, even in women who received treatment at the age of 55 years or younger.”
For more information on the strengths and weaknesses of this study and a discussion of whether hormone replacement therapy might be right for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
___________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance