Why Does Supplementation Matter During Hospitalization?
Author: Dr. Stephen Chaney
 I have often said that age doesn’t necessarily bring wisdom, but it does bring perspective. When I first started teaching medical students in the early 70’s, the idea that optimal nutrition was important for hospitalized patients was new and exciting.
I have often said that age doesn’t necessarily bring wisdom, but it does bring perspective. When I first started teaching medical students in the early 70’s, the idea that optimal nutrition was important for hospitalized patients was new and exciting.
A series of groundbreaking papers documented that many patients, especially elderly patients, were in poor nutritional status when they entered the hospital. For these patients optimizing their nutrition while they were in the hospital and shortly thereafter:
- Reduced mortality and increased recovery from whatever treatment they were undergoing.
- Reduced the incidence of sepsis (systemic infection) and other severe side effects of the treatment.
- Reduced recovery time in the hospital.
- Allowed them to return to their normal daily activities more quickly after they left the hospital.
Those discoveries revolutionized medicine. Every hospital now provides tube feeding and iv infusions for very ill and nutritionally compromised patients. And these innovations have improved the effectiveness of hospital care.
So, when I saw a recent paper (GE Baggs et al, Clinical Nutrition, 42: 2116-2123, 2023) with the title “Impact of a specialized oral nutritional supplement on the quality of life in older adults following hospitalization”, my initial thought was this was old news.
But then I read further. You see, feeding tubes and iv infusions are very effective. But if you or a loved one has ever been hospitalized for a serious illness or accident, you also know they are very expensive.
When I read this study, I realized they were talking about a less expensive option, the equivalent of providing these patients with a multivitamin and a protein shake providing certain critical nutrients. That got my attention.
How Was This Study Done?
 This study utilized data from something called the NOURISH [Nutrition effect On Unplanned Readmissions and Survival in Hospitalized patients] trial. This trial enrolled hospitalized older adults with malnutrition. As the title of the trial suggests, this study tested the effect of the nutritional intervention I will describe below on unplanned readmissions after hospitalization (which you want to be as low as possible) and survival after hospitalization (which you want to be as long as possible).
This study utilized data from something called the NOURISH [Nutrition effect On Unplanned Readmissions and Survival in Hospitalized patients] trial. This trial enrolled hospitalized older adults with malnutrition. As the title of the trial suggests, this study tested the effect of the nutritional intervention I will describe below on unplanned readmissions after hospitalization (which you want to be as low as possible) and survival after hospitalization (which you want to be as long as possible).
That study reported that hospitalized patients who received the prescribed supplement experienced:
- Improved nutritional status.
- Improved survival and reduced readmission after leaving the hospital.
This study re-analyzed the same data set to determine whether the same patients also experienced improved quality of life. Here are the specifics of the study:
Elderly (average age = 78) patients who were recently admitted to the hospital with a diagnosis of congestive heart failure, acute myocardial infarction (heart attack), pneumonia, or COPD were screened for nutritional status. From this group, 622 patients with moderate or severe malnutrition were selected for the study. Patients with this combination of age, severe cardiopulmonary disease, and poor nutritional status generally have poor outcomes and increased risk of readmission.
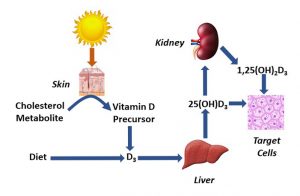
The patients were randomly split into two groups. One group received standard care. The second group received a beverage containing 20 grams of protein, 1.5 grams of beta-hydroxy-beta-methylbutyrate (HMB), plus vitamin D and other essential micronutrients.
[Note: HMB is a metabolite of the amino acid leucine. And, like leucine, HMB stimulates an increase in muscle protein synthesis, reduces loss of muscle mass during hospitalization, and enhances the regain of muscle mass during recovery. HMB and leucine give essentially equivalent results.]
The second group received a placebo beverage containing 12 grams of carbohydrate, 10 mg of vitamin C, but no protein, HMB, or other micronutrients.
Patients were instructed to drink 2 servings of the beverage a day during hospitalization and for the first 90 days after discharge from the hospital.
On the day they were discharged from the hospital (day 0) and on 30, 60, and 90 days after discharge the patients met with trained coordinators who administered questionnaires assessing their quality of life.
Is Supplementation Important For Hospitalized Patients?
 When compared to the placebo, the supplement described above provided significant improvements in:
When compared to the placebo, the supplement described above provided significant improvements in:
- General health on days 0, 30, 60, and 90 after leaving the hospital.
- Mental health on days 60 and 90 after leaving the hospital.
- Vitality and social functioning on day 90 after leaving the hospital.
In addition, there was a trend towards improvement for:
- Physical functioning, reduced body pain, and mental health-related role limitations [for example, taking care of a spouse].
The authors concluded, “Among malnourished, hospitalized patients (aged ≥ 65 years), supplementation with S-ONS [their acronym for the supplement used in this study] during hospitalization and 90 days post discharge resulted in improved quality of life. These benefits complement survival benefits previously shown in the NOURISH trial analysis.”
Why Was This Supplement Effective?
 You will notice that the beverage used was relatively high in protein (20 grams) and included added HMB to help increase muscle mass. It also contained a variety of micronutrients.
You will notice that the beverage used was relatively high in protein (20 grams) and included added HMB to help increase muscle mass. It also contained a variety of micronutrients.
There are two reasons for this design.
- You have heard the saying, “It’s all downhill after age 30.” With muscle mass the downhill slide starts around age 50. This age-related loss of muscle mass is referred to as sarcopenia.
Sarcopenia can be slowed by resistance training plus diet or supplementation that provides around 20 grams of protein plus either leucine or HMB 2-3 times a day.
However, many older adults have trouble fixing healthy meals and end up protein and micronutrient deficient.
- Severely ill patients enter what is referred to as a catabolic state. They break down their muscle and energy stores at a high rate. This is also true for patients recovering from major surgery or trauma.
The catabolic state dramatically increases protein and calorie needs just to prevent the body from cannibalizing its own tissue. Again, previous studies have shown that a protein supplement providing around 20 grams of protein and either HMB or leucine can slow this process.
What Does This Mean For You?
 There are two major take home lessons from this study.
There are two major take home lessons from this study.
1) Who needs supplementation?
I have covered this topic in previous issues of “Health Tips From the Professor”, but let me summarize the key points here.
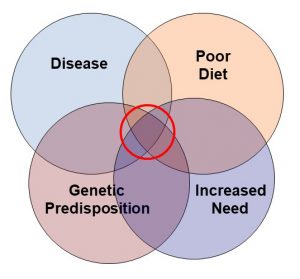
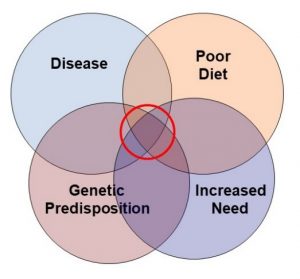
- Supplementation can fill the gaps in an inadequate diet. Multiple studies have shown that most Americans get inadequate levels of one or more essential nutrients from their diet. And restrictive diets ranging from vegan to keto create additional nutritional deficiencies.
-
- And, for this purpose, supplementation need not be complicated. A multivitamin and a plant protein shake to replace some of the animal protein in the typical American diet would suffice.
- Supplementation can reduce the risk of certain chronic diseases. We should not think of supplementation as a “magic bullet”, but I do recommend it as part of a holistic approach to wellness.
-
- In this case supplementation starts with a protein shake and a multivitamin, but often includes targeted nutrients such as omega-3s.
But this study reminds us of another key point about supplementation.
- We should supplement before we need it most. The seniors in this study were already “behind the 8 ball” when they were admitted to the hospital because they were malnourished – something that likely could have been prevented with a simple program of supplementation and exercise.
This is a lesson that applies to all of us.
-
- Chronic diseases like high blood pressure, diabetes, and cancer “sneak up on us”. They often develop years before we or our doctors recognize them. Studies show that diet and supplementation reduce the risk of developing these diseases, but they are much more difficult to reverse once you have them.
-
- Most hospitalizations are unplanned. And if we enter the hospital with optimal nutritional status, the outcome of our treatment is much better than if we enter the hospital in poor nutritional status.
-
- Colds and viruses strike without warning. We are much more likely toward them off or recover more quickly if we are in good nutritional status when we are exposed.
2) What kind of supplement do we need? Don’t misunderstand me. There are times when tube feeding and iv infusions are absolutely essential for some hospitalized patients.
But this study showed that a well-designed protein supplement containing the essential micronutrients was sufficient for most elderly, malnourished patients hospitalized with severe cardiopulmonary diseases.
- The formulation used in this study was produced by a pharmaceutical company. However, any high-quality protein supplement providing 20 grams of protein with added leucine or HMB plus a multivitamin supplement should provide the same benefits at a lower cost. The multivitamin could be in tablet or powder form.
- The catabolic state associated with hospitalization also increases energy requirements. The protein supplement used in these studies had 350 calories and 44 grams of carbohydrate.
Most commercial protein supplements are designed for weight loss or weight maintenance and have fewer calories. So, for hospitalized patients extra calories would need to be provided in the form of foods containing healthy carbohydrates and fat.
The Bottom Line
Recent studies have shown that providing elderly, malnourished patients with a simple, inexpensive supplement regimen during and following hospitalization leads to better outcomes and better quality of life for the hospitalized patients. These findings illustrate two important concepts about supplementation:
- The time to supplement is before you need it. Most hospitalizations are unplanned, and your outcome will be much better if you enter the hospital in optimal nutritional status.
- Supplementation need not be complex and expensive. The supplement regimen used in this study is equivalent to a high-quality protein supplement with added leucine or HMB plus a multivitamin.
For more details about these studies read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.